Author:
Dr. Mukta Mahajan, Consultant – Radiologist Breast Imaging and Intervention
India is experiencing an unprecedented rise in the number of breast cancer cases across all sections of society, accounting for 27% of all cancers in women, less than 10% of which are inherited. India also has far lower survival rates of 66.1% for breast cancer compared to 90.2% in the USA. There are several stark differences for this disease in India and the West.
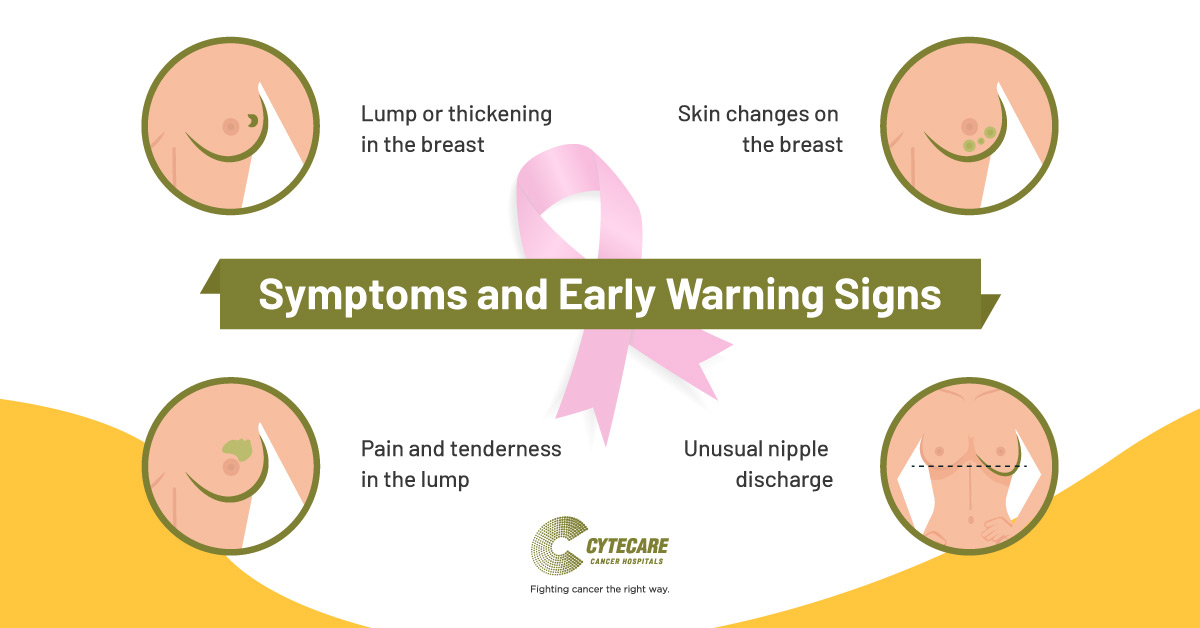
Indian women often develop the more aggressive subtype of cancer at a much younger age. At the time of detection, the cancer is often in an advanced stage resulting in more aggressive treatments and poorer outcomes. Lack of nationwide screening program makes detection of early curable breast cancer even before the development of any symptoms an unrealistic goal. Even among the educated or the urban population, only a few are aware of the early signs and breast cancer symptoms.
Attention to routine self breast examination as well as by trained medical personnel is still dismal. Lack of expertise, misconceptions about mammography and biopsy further decrease the chances of timely detection. These, along with a general indifference towards women’s health, financial constraints and social stigma increase the hurdle to effective treatment.
On a brighter side, when detected ‘early’ breast cancer is curable, needs less aggressive treatments, has a lesser psychological impact and certainly has a far lesser financial and social burden on the family. Small scattered efforts to empower women to be “breast-aware” through simplified information are picking up pace. The need for routine examinations, improved access to trained personnel at a community level and quick referrals to specialized centers is being realized.
Breast Cancer Detection Techniques
Primary breast examination or screening is done to identify the presence of any cancerous mass. Common breast cancer detection techniques include:
- Breast Examination by the doctor
- Mammography
- Breast Ultrasound
For a confirmed diagnosis and to identify the stage of cancer, the patient might be required to undergo other diagnosis tests like a biopsy and other imaging tests like Breast MRI.
What methods are used for early detection of breast cancer?
The early breast cancer detection methods include screening mammography and clinical breast examination.
Mammography is the most often used, best breast cancer detection method. It uses low energy X-rays for a human’s breast cancer screening and diagnosis. Early breast cancer detection is essential for an effective cure for the disease.
What to expect during a visit to a breast clinic?
A woman with a breast complaint will have a physical examination followed by appropriate tests suited for her age and seriousness of her symptoms. Mammogram (preferably 3D digital mammogram) and ultrasound are the initial steps of assessment of any suspicious breast symptom. Breast radiologists expedite breast biopsies in these patients to confirm the presence and type of cancer. An image-guided breast biopsy is a highly accurate, minor, almost painless OPD procedure and requires little preparation from the patient. No special care is required after the biopsy, and the woman can resume her daily schedule the same day. The biopsy results are ready within a few days for further discussion regarding treatment.
A woman without any breast complaint between the ages of 40-75 years can self-refer herself for an annual screening mammogram to look for early signs of breast cancer. If someone is younger but concerned, a consultation with a trained breast radiologist or surgeon can help to assess if there is a higher risk of breast cancer and tailor the screening tests according to the risk profile.
Do all breast lumps need to be surgically removed?
Most breast lumps are fortunately non-cancerous. This can be confirmed easily on a mammogram and/or the ultrasound. A small subset of these lumps needs further assessment with simple core biopsies to confirm their benign nature. Benign, i.e. non-cancerous lumps don’t need surgical removal. It is important to mention that the role of rampantly performed needle test known as FNAC in breast diseases is long gone and now only reserved in remote primary health centers with limited-resources. Core biopsy has become the minimum standard of assessment. There has been a steady improvement in the yield, accuracy, and negative predictive value of minimally invasive breast biopsy procedures through newer sophisticated techniques such as vacuum assisted breast biopsy or VABB.
More on VABB
The entry of VABB in clinical practice has been a game-changer. It is an accurate one-step OPD procedure that has simplified diagnosis of paucicellular breast cancers and even precursors of breast cancer that earlier needed admission, general anaesthesia and surgery. It is performed in a radiology suite with the help of ultrasound, mammogram or MRI. Suspicious areas of any size and depth can be accurately targeted using a mechanized VABB needle-suction apparatus. Needle position is guided and confirmed by a radiology scan followed by withdrawal of a series of large samples across 360 degrees rotation through a single needle entry.
VABB reduces underestimation of cancerous disease, re-biopsy rates, number of surgeries and overall cost burden for women with cancerous lumps. VABB has the potential to diagnose and even treat benign diseases that cause bloody or watery nipple discharge without missing a hidden cancer. Its role in certain small non-cancerous lumps is also worthy of mention since VABB can avoid surgery, scarring and disfigurement of breasts. Compared to surgical excision, VABB shows significantly lower rates of operative and recovery times, blood loss, as well as wound infections. There is adequate evidence of safety and efficacy of VABB in diagnostic biopsies as well as excisions of small benign lumps such as fibroadenomas. VABB has been approved by the FDA (USA) as well as NICE (National Institute for Health and Care Excellence, UK). VABB has consistently shown high satisfaction and lowest pain perception on several patient surveys.
How do breast radiologists contribute towards improving breast cancer outcomes?
Breast radiologists are a part of the core team of multidisciplinary cancer care of pathologists, surgeons, medical and radiation oncologists as well as pain and palliation specialists. Breast radiologists receive specialized training in screening, diagnosis, staging and response assessment tests as well as minimally-invasive procedures. Misdiagnosis of cancer and false assurance of wellness is a missed opportunity for all of us to save lives. Avoiding such delays needs continuous education, review and improvement of our services. Breast imaging society of India is setting the ground by standardizing practice guidelines and quality assurance measures for the centres that offer these services.