
Author:
DR. VASUDHA N.R, Associate Consultant – Paediatric Oncology
Acute Lymphoblastic Leukaemia (referred to as ALL) or commonly called blood cancer, is the most common cancer in childhood.
Being faced with a diagnosis of blood cancer in your child can be a gruelling experience. When faced with this dreaded diagnosis, parents and caregivers often find themselves alienated in a world of complex terms, medications, and instructions. Understanding the underlying problem can not only empower the caregiver but also restores a sense of calmness and courage, which is required to face the next few months of treatment for Acute Lymphoblastic Leukemia or blood cancer.
The term Leukaemia is derived from the words (Leucos + haima), which roughly translates into an excess of white blood cells in the blood. In simple terms, Leukaemia is a cancer of white blood cells.
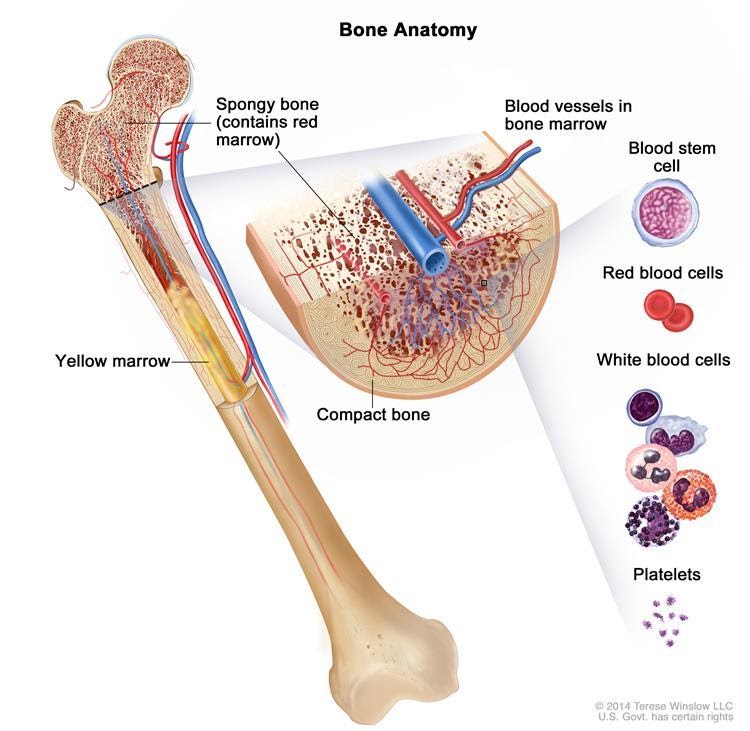
Before we understand more about blood cancer, it is important to understand the bone marrow’s functions, which is the primary blood-forming tissue. The bone marrow is the soft spongy tissue in the centre of the bone, which produces different types of blood cells that are required for diverse functions in the body.
As illustrated below, the bone marrow produces white blood cells that provide immunity, platelets that control bleeding, and red blood cells that carry haemoglobin and, in turn, transport oxygen.
What Happens in Blood Cancer?
Leukaemia or blood cancer results from the unregulated proliferation (multiplication) in white blood cells. This process results from a genetic change/aberration in a single cell’s DNA due to as yet unknown reasons. In a child with blood cancer, the bone marrow is unable to produce normal cells and instead produces a surplus of abnormal cells called blasts, which eventually takes over the bone marrow.
These are immature cells that divide uncontrollably and replace the normal components of the bone marrow, namely red blood cells, healthy mature white blood cells and platelets. Simply speaking, this scenario is akin to a garden full of weeds that steals the nutrients and does not let healthy plants grow. Hence children with ALL have lower than normal numbers of red blood cells (anaemia), white blood cells (neutropenia) and/or platelets (thrombocytopenia).
What Causes Blood Cancer in Children?
This is a question that haunts most parents and caregivers who often wonder “what they did” or “what they did not do” caused cancer. Unfortunately, in almost all childhood cancers, including blood cancer, there is no apparent cause that can be singled out. A small minority of cases are associated with inherited genetic syndromes, such as down syndrome.
It is known that exposure to high levels of radiation increases the risk of developing blood cancer.
Several causes like exposure to pesticides are postulated for the causation of Acute Lymphoblastic Leukemia, however, none of these has been proved across various studies. There is some evidence blood cancer could be linked to common childhood infections.
One important point to note is that Acute Lymphoblastic Leukemia (ALL) is not infectious; it cannot be passed on from or to other children with ALL.
Symptoms of Blood Cancer
The most common symptoms of blood cancer in children are caused due to changes in the bone marrow and manifest with fever (high temperature) due to infections and impaired immunity.
Excessive pallor and fatigue (extreme tiredness) due to anaemia and excessive bruising or bleeding. The bruising is of concern when it occurs in areas not susceptible to blunt trauma, for example, on the chest, abdomen, face, etc., and bleeding is of concern when it happens easily with no trauma, such as bleeding from the gums when brushing their teeth.
In addition, children may have swelling of their lymph nodes or lymph glands. Sometimes, children may have bone or joint pains, and, in very young children, this may present as a reluctance or inability to bear weight in a previously well child.
All of the signs or symptoms of blood cancer described are quite common in children. It is very rare for a child with these symptoms to be found to have a serious disease.
How is Blood Cancer Diagnosed in Children?
There are several tests that are carried out to confirm a diagnosis of blood cancer in children. The first step towards diagnosis of a suspected child with leukaemia is a Full blood count. A full blood count, also called the complete blood count, is a blood sample examined using an automatic cell-counting machine and looking at a stained film of blood under a microscope. If your child has blood cancer, the cell counter will usually indicate large numbers of abnormal white cells in the blood. However, it is important to understand that in rare cases, the blood count may be normal or lower than normal.
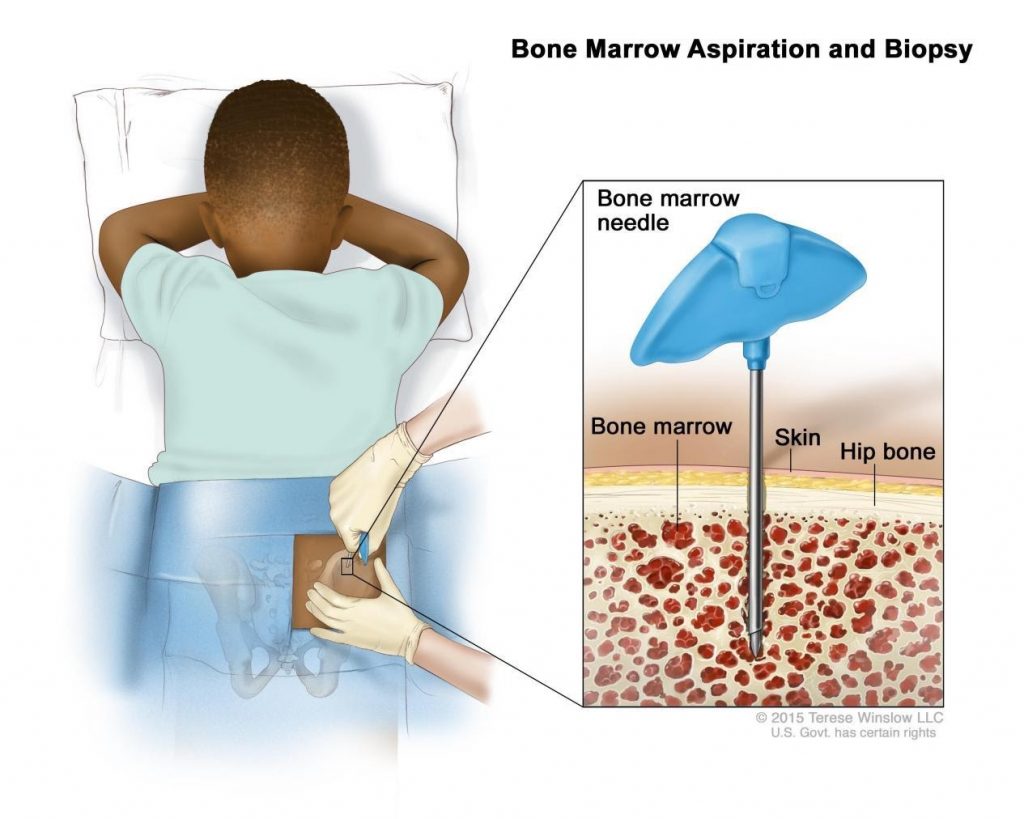
The second and most important step in further confirming the diagnosis of blood cancer in children is a bone marrow examination. This is a minor procedure usually done under general anaesthetic or sedation for younger children and local anaesthesia for older children. It does not take very long. Bone marrow examination is done with a bone marrow needle, and samples are usually taken from the pelvis bone. Your child may have some pain and soreness in the bone marrow aspiration site, which will subside in a day or two.
Additional investigations called Flow cytometry and Cytogenetics help doctors classify and stratify the child’s disease to deliver the appropriate therapy.
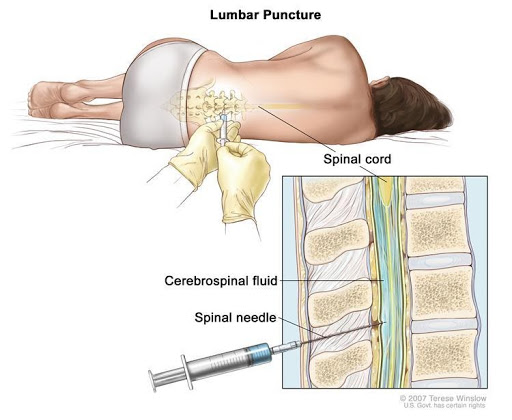
CSF Analysis: During the evolution of treatment for blood cancer, doctors learnt that blood cancer or acute lymphoblastic leukemia (ALL) cells could sometimes get into the fluid around the brain and spinal cord (cerebrospinal fluid or CSF). For this reason, at diagnosis, a sample of the CSF is tested to look for leukaemia cells. This is called a lumbar puncture and, like bone marrow sampling, is usually done under local anaesthetic and sedation in older children and a general anaesthetic in younger children.
Treatment of Blood Cancer in Children?
Chemotherapy is the mainstay of treatment for blood cancer in children and is given in specific phases or blocks (often called a protocol or regimen). Chemotherapy aims to kill the leukaemia cells and enable the marrow to function properly. Combinations of different drugs are given in an intensive phase that lasts for 6-7 months, followed by a maintenance phase that lasts for 2-3 years. In addition to chemotherapeutic agents, steroids are also an integral part of the treatment of blood cancer.
After the first phase of blood cancer treatment, it is important to assess chemotherapy responses, which will again be evaluated with a bone marrow examination.
During the course of blood cancer treatment, a lumbar puncture and intrathecal chemotherapy similar to that done at diagnosis will have to be repeated at regular intervals.
Is a Bone Marrow Transplant Required for all Children with Blood Cancer?
In the setting of a primary disease (first time), a minority of children who do not respond well to chemotherapy or those with a high-risk cytogenetic profile will be considered for bone marrow transplantation. The majority of children with ALL can be completely cured with chemotherapy alone.
SOURCES:
- Childhood Acute Lymphoblastic Leukaemia (ALL); A Guide for parents
- www.leukaemiacare.org.uk
- Children and Young People with Cancer / A Parent’s Guide / Acute lymphoblastic leukaemia (ALL) www.cclg.org.uk
- www.cancer.gov


